Celebrating Over Six Years
0 Comments
Celebrating Five Years
Celebrating Four Years
Celebrating Three Years
Celebrating Two Years
Celebrating One Year MarkLooking back, it seems like it was a long time ago when I was diagnosed with breast cancer on March 23, 2017 followed by a double mastectomy on May 10, 2017. The following four sessions of chemo in July and August went about as well as they could. (Read previous posts for the specifics.) I managed twenty-eight daily sessions of radiation in October-November without getting burned or having excessive fatigue. However, I’m sure that many of these memories are fading, which is a good thing.
Since my cancer type was Estrogen Responsive Positive (ER+), and all the other types negative, I need to take an anti-estrogen medication for 5-10 years. The Aromatase Inhibitor I have started is Letrozole. It is one of three types in this class of drugs, and so far I have not experienced any adverse side effects other than HOT FLASHES. Wow, I thought I was done with them long ago. Fortunately, they don’t come too often or last too long. I am also happy to report that in February-March I was back teaching classes at the Green Valley Camera Club. When we returned to Portland, I took advantage of some photo opportunities that included tulip fields and a walking iPhone class offered by Apple. We also attended a Timbers soccer game when the Providence Cancer Institute provided me and fellow survivors with four tickets. We enjoyed the company of our friends Alberto and Shannon. I have now passed the one year mark, and have seen all my appropriate doctors. They have all given me a good report. I see my oncologist, Dr. Acheson, in six months and the others in a year. To celebrate, I plan to do the Komen “Walk” for the Cure here in Portland on September 16, 2018, and am hoping some of my friends will join me. We will also be back to doing some traveling this summer, so watch for posts about eastern Canada on my Travel Blog. Thanks go to my many friends who have been so supportive through this whole experience. That is all for now as I am back to a normal life and hoping that my motto of “No Regrets,” where I did everything recommended, will pay off. Grace End of Radiation and On With Life! Wow, what a year 2017 has been. It definitely had its high and low points, but the good thing is that it is ending on the up side.
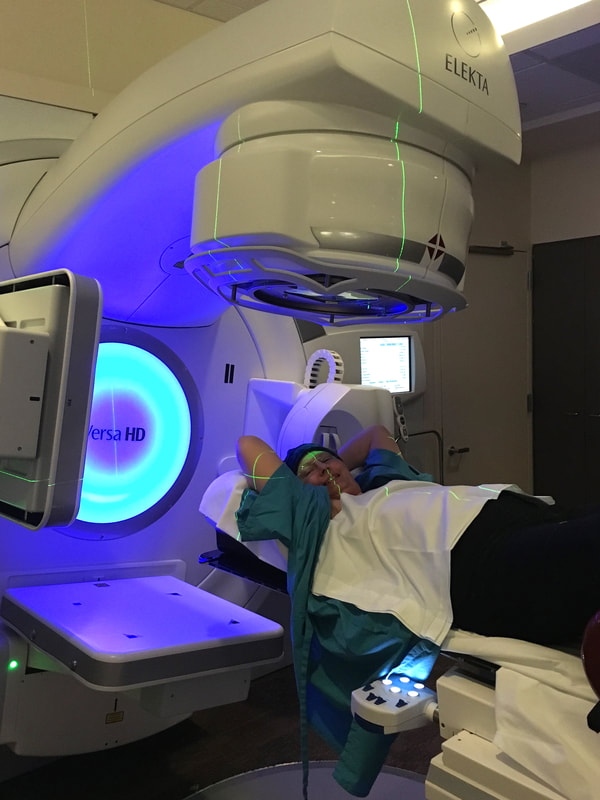
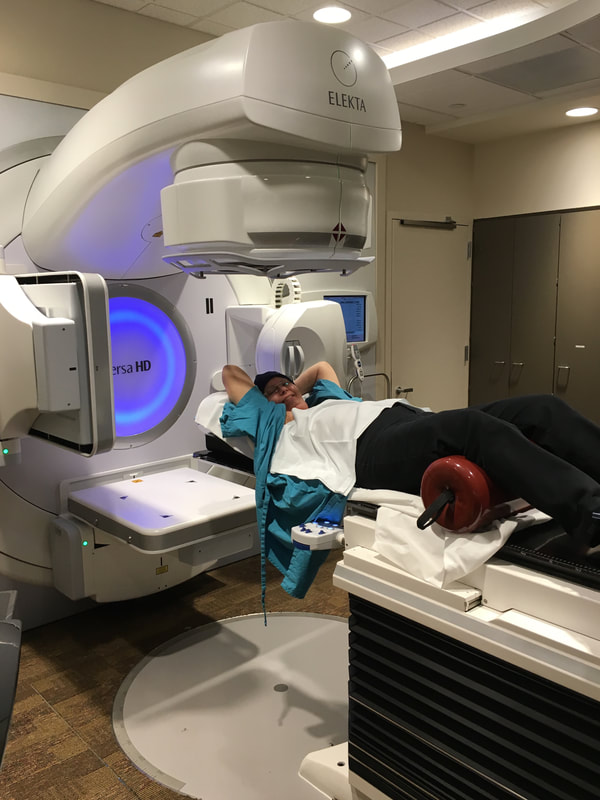
To do a brief recap: the year started with our going to Green Valley, AZ in January followed by a two week trip to Cuba in February. That was when I discovered a lump in my armpit. The end of March I had it biopsied and it was diagnosed as a lobular carcinoma. Since we were scheduled to leave in two days for a two week photo expedition cruise around Baja, California, we were encouraged to go. It was a great distraction. (See photos under Photo Gallery menu above.) We returned to Green Valley then home to Portland in mid April when the whirlwind started. An MRI showed that I had several tumors in the breast on the other side, which the 3-D Mammogram did not show. So, on May 10 I had a double mastectomy. My cancer type was Estrogen Responsive Positive (ER+) and the Oncotype DX test showed that I would benefit from Chemo. I started the four sessions of chemo on June 28 and the last session was on August 31. I managed the side effects, which you can read about in previous posts. In October 13 I started radiation treatments. They were daily for 28 sessions, ending on November 20. (My November 4 Post tells the details of the sessions.) There were a couple of side effects. One was fatigue. Since I was already back to working out at Curves three days a week and walking three days, I found the fatigue minimal. The other effect was like a “sun burn.” I managed to keep that to a minimum by using two gels: Aloe Vera 99% and Calendula three times a day. After the last treatment I was given a prescription for 1% Silver Sulfadiazine Cream which is used on burns. I applied it thickly twice a day. Dr. Gannett, my radiation oncologist was always pleased with how well I was doing. I saw him on December 18, one month after my last treatment, and should not have to see him again. Meanwhile, on November 29 I met again with Dr. Acheson, my medical oncologist. She was pleased with how well I am doing. We had a discussion about what comes next. My type of breast cancer is Estrogen Responsive Positive (ER+.) This means it feeds on estrogen. Believe it or not, our bodies continue to produce estrogen after menopause, so it is important to shut down all of it. Therefore, there are various medications that are recommended to reduce the risk of the cancer re-occurrence. Since I do not have a bone density problem, I qualify for the class of drugs called Aromatase Inhibitors (AI.) Dr Acheson is starting me with Letrozole. It is important to be able to take one of these for at least five years. If I tolerate this one, great, if not there are two other AI drugs to try. I started December 1, and so far so good. Then there is my hair. It has now grown out to about an inch long. I can tell there will be some curl, at least for a while. It will be some weeks before I stop wearing something, hat, scarf or wig, because I’m cold otherwise. Then there is my heart issue: totally unrelated to my cancer. I continued to have occasional AFib episodes. I had a 48 hour Holter Monitor test which showed no pauses over 2 seconds. I also had an echo stress test (with treadmill) which shows my heart muscle is healthy. All Good News!!! Since I’m on the blood thinner Eliquis I don’t have to worry about blood clots and strokes, so until my AFib episodes get to be too frequent or of concern, I don’t need to have anything done about them. It is good that I have two cardiologists looking after me. About the time I started chemo I learned about the Breast Cancer Support Group sponsored by Providence St. Vincent, which meets twice a month. I have attended all but one session since then, and find them very helpful. I have been able to learn from others going through what I have, am or will go through. The women who run the sessions are also very helpful, and I plan to continue attending when I can. So, this ends the year 2017, and I’m so thankful that I have made it through all of these annoyances and blips to my health. I’m looking forward to the new year and getting back to “normal.” We look forward to returning to Green Valley, AZ for the winter where I have twelve classes already scheduled for me to teach at the Camera Club. I will post again in the future every once in a while to chronicle any changes, or to just let you know I’m doing fine. You can also check back periodically to see photos of our travels. That was the original purpose of my website, since travel and photography are my special interests. Until then, thanks for reading about my breast cancer journey. I hope it has been informative. May we all have a Happy New Year! Grace Thank You: From My Sister Dear Special Friends of Grace,
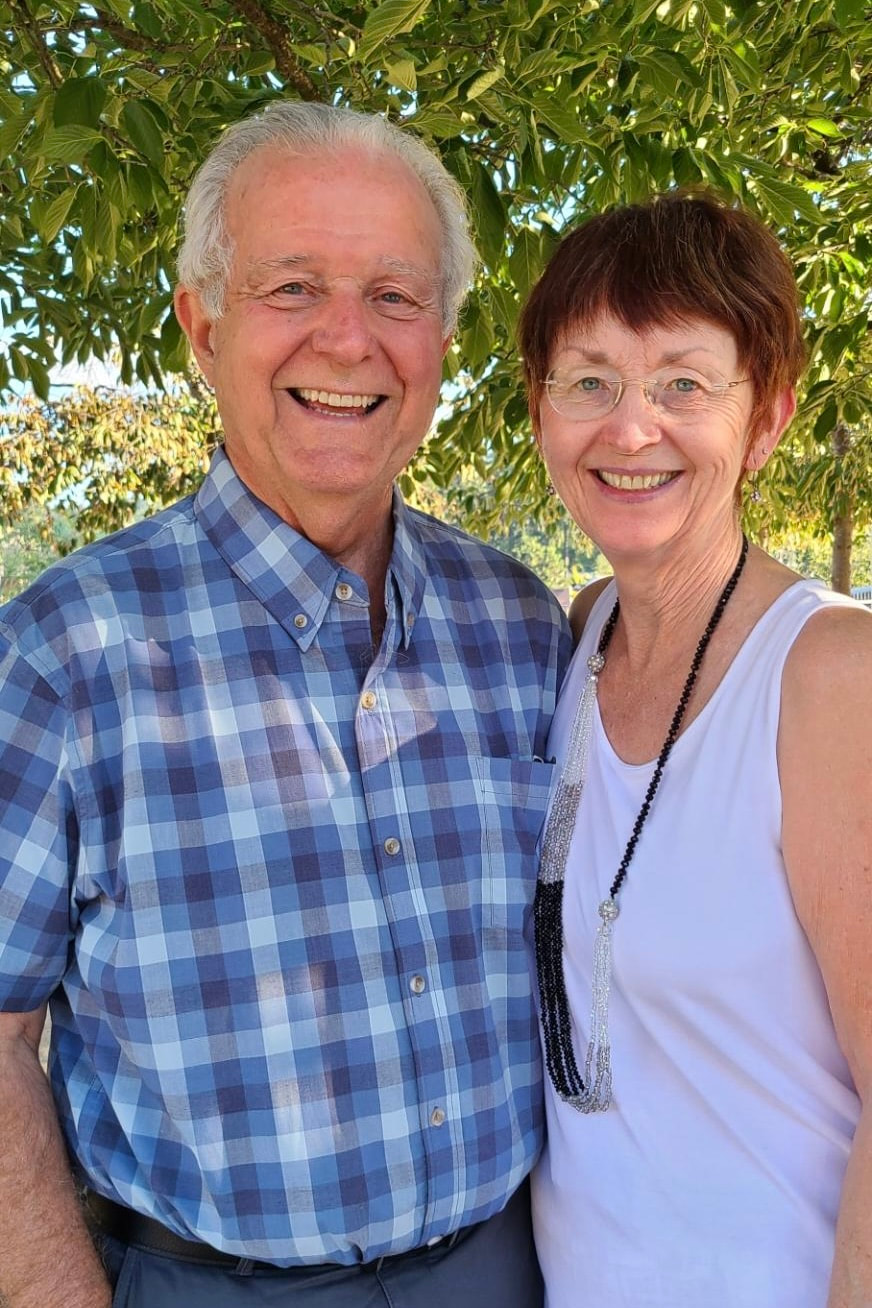
Grace is my older sister. We've been together for many years ;0) She means the world to me. I would prefer to be the one to do all the things for her that I will mentioned. Since it was impossible for me to do all that, along came you folks, "Grace's Special Friends". "Thank you!" to each one of you for coming along side her, cheering, comforting, and doing whatever you did, to make her year bearable, enjoyable at times, and doable because you were there for her. I deeply appreciate what you have done and wanted you to know my observations as time went by and Grace's sense of well-being because you were there for her. This is Grace's last week-end before her last Radiation treatment, and then there is "recovery time." Some of you were with her from the beginning, making trips to the doctors, and taking notes which relieved her mind so she could focus on what was being said. Some of you took on the "Care-Giver" role. Some of you periodically provided transportation. Some of you cooked special meals, and brought them over for Paul and Grace. Some of you sent her flowers, cards, and your prayers and love. Some chose to wait in the waiting room during her surgeries. I know that Paul appreciated your support, as well. Some called to see how she was doing; and, my guess is, some of you checked on Paul to see how he was doing. I'm sure I left out some of your acts of kindness toward Grace. Grace is a wonderful sister to me and a great example for me to follow on this road of recovery. May each of you stay in good health for many years to come; and if not, may you be surrounded by the same kind of friends that you have been to Grace to help see you through. May God bless you as you have blessed others. Very Sincerely, Gayle Radiation: First Half of 28 Sessions I see that my last update was dated September 20, which seems like a long time ago. It was three weeks after my last chemo infusion. Since then all of my side effects have disappeared with the exception of my fuzzy/numb feeling toes. My strength has slowly returned and a couple weeks ago I realized that I really was feeling very NORMAL. For three weeks now I have been back to doing full workouts at Curves, three days a week, and walking the other three days of the week. This is all very good since fatigue is a normal side effect of radiation and so far, I have not experienced any!
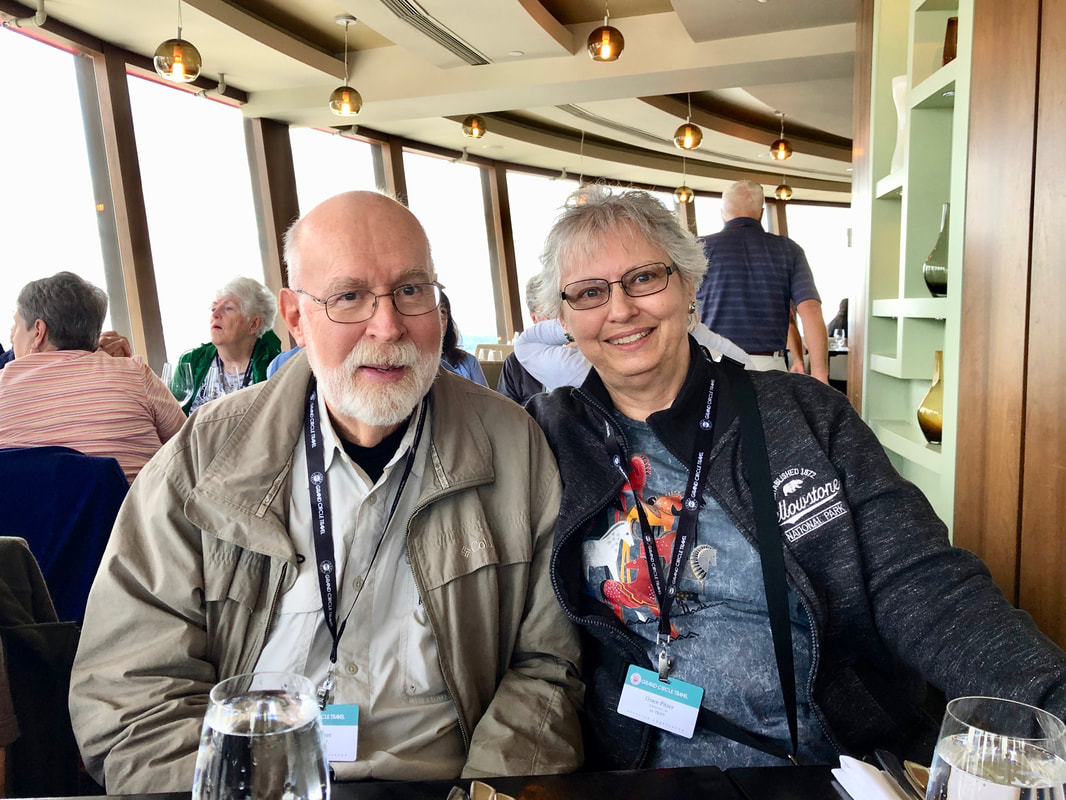
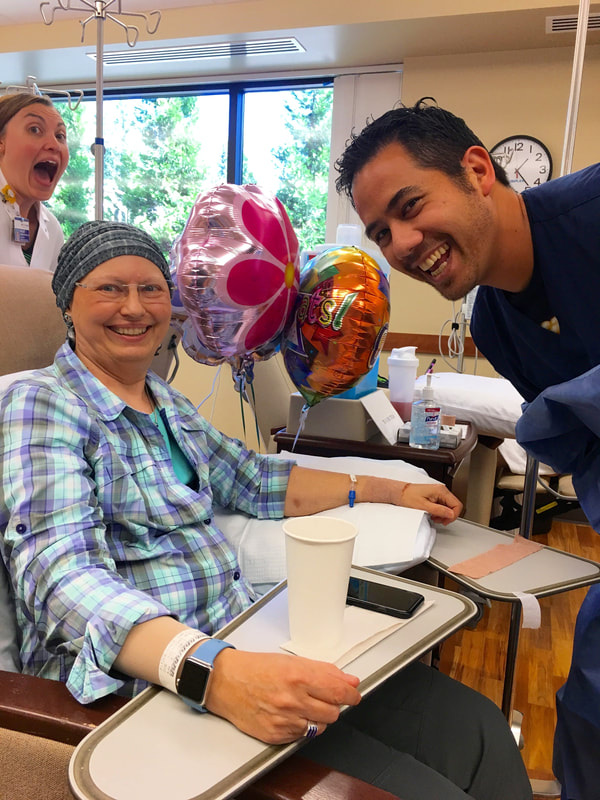
On October 3, I had the “mapping” for my radiation treatments. They made a mold of me in the right position so I can lay in it exactly the same each time. I started the 28 daily sessions on October 12. My regular appointment is 10:24 AM every day. I always go in early, just in case traffic is bad, and work on the group jigsaw puzzle they make available. The actual session only takes less than ten minutes, and the radiation from three angles is for 12, 10 and 19 seconds each. About day 12 my skin started to get a little pink. I have been faithfully using the recommended 99% Aloe Vera gel and Calendula gel three times a day. This is when it may be an advantage that much of the area is still numb from the surgery, so I’m not feeling many uncomfortable sensations. Every week they take X-Rays of me in position to make sure everything is still being set up correctly. Once a week I also see Dr. Gannett. He answers any questions I have and looks at my skin to see how it is fairing. So far, he is very pleased with how everything is going and how good my skin is tolerating the treatment. He is also surprised that I am not yet experiencing any fatigue, but attributes that to my continued exercising. One thing I learned in our discussion is that the side effects (fatigue and skin irritation) should be gone within three weeks of ending the radiation treatments. November 20 is the last one, so that means I should be in good shape by the second week in December, if not before. Also, my hair is growing back, but can still be measured in 1-2 mm. I'm trying to be patient and know it will take a couple more months to be presentable. In the mean time, my warm fleece stocking caps will have to do. On November 29 I meet again with my medical oncologist, Dr. Acheson, to discuss the anti-estrogen pills I will need to take for at least five years. I expect I’ll be starting them in early December. That can be the next blog post topic. It has been fifteen years since we have remained in Portland for the fall season, to enjoy all of the gorgeous foliage colors. We have missed that, so we are really enjoying colorful trees and the nice weather we have also had, up until this week. The rain has now hit. That doesn’t stop me from my walks, however, as I have plenty of rain gear. I finally did put a personal post on Facebook in honor of “Breast Cancer Awareness Month” to encourage everyone to get those annual mammograms. And, if the results come back with a “Too dense to be sure” comment, have a followup ultrasound, at least. I’ll make another update when the radiation is finished (11 more to go) and the extra three weeks the side effects could last. Happy Thanksgiving. Paul and I certainly have a lot to be thankful for; especially my getting back to good health!! Chemo: Session Four - THE LAST, August 31, 2017 On August 31 I had my LAST of four chemo infusions. Besides Paul, I was joined by my friends Melanie and Sarah. Melanie even brought balloons and cupcakes to celebrate the occasion. After my blood draw I met with Erin, the physician’s assistant, who reviewed my last three weeks, checked me over, and discussed any possible changes for the next three weeks. She did mention that the results of chemo is cumulative and the fourth could hit me a little harder. My blood work was good, so we all moved to the infusion room. Since it was lunch time by then, I sent everyone off for lunch while I took the Zofran anti-nausea pills and ate my own peanut butter and jelly sandwich along with some things I scrounged from the refrigerators. After the half hour wait for the Zofran to take affect I was hooked up to the Taxotere bag which took an hour to empty. Sometime during that hour everyone came back from lunch. Paul figured I was in good hands, as Melanie could take me home. Before he left, we got a group picture of my three supporters for the day. (see below) When it was time to switch to the Cyclophosphamide bag, which only required a half hour to empty, Sarah took a picture of me with my nurses for the day. (see below) They were all excited for me that this was my last visit. I was pleased that my friends cared enough to spend the time with me. However, I knew this wasn’t the end!!! I still had to endure the three plus weeks of side effects from the final chemo infusion. As I mentioned above, I was told the effects were cumulative, and she was right. They hit harder and faster. 1. Fatigue: Started Day 2 and I noted it was serious until Day 12 when it let up some and came back Day 18 and continues on to Day 21. Hopefully it will not last much longer. 2. Nausea: I took Compazine for nausea on Days 1, 2, 4, 5, and 9, mostly at night. I would take it if my stomach was even a little unsettled so I really never got sick. 3. Tender fingernails: Started Day 5 and lasted until Day 13. My thumbnails are growing out with ridges parallel to the cuticles and all my fingers have vertical ridges. They are very brittle so I keep them fairly short. 4. Feet: About Day 11 I realized my feet felt like I had on very fuzzy socks. When I looked, there were no socks. This has persisted until now, some days more so than others. Sometimes the soles of my feet have spasms, which don’t last long. This was a new side effect. 5. Mouth Sore: Starting Day 4 my tongue became sore, mostly the edges. By Day 6 the texture on the roof of my mouth became rough. This lasted at least a week or so. I rinsed with salt water to help. 6. Taste Changes: The sore mouth coincides with how things taste, including water. Food and water didn’t start tasting normal until after Day 13 and I noticed water tasting normal on Day 18. Finally I can enjoy eating and don’t mind drinking. 7. Atrial Fibrillation: I speculate that because of my extreme fatigue, staying on the sofa, and water not tasting good, I let myself get dehydrated. The night of Day 11 my heart went into AFib, which I noticed after I went to bed. I got up and took my blood pressure, which was low, and my heart rate was 101 bpm. I used my Kardia EKG device that connects to an App on my iPhone and took a 30 second reading, which confirmed my suspicion. I printed it for my records, drank some water and went back to bed. In the morning I started downing Gatorade for the electrolytes, and by noon my heart was back in normal rhythm. This left me even weaker, however. (See below titled “Living With AFib” to learn about this little EKG device and the App.) 8. Imodium: I only needed to use it once, on Day 11. 9. Prunes: I discovered they are my friend and almost daily consumption kept me from needing to use any Dulcolax. On Day 11, September 10, we had to miss a family wedding because of my extreme fatigue. It was later that night when the AFib started. The next evening I had to miss my Delta Kappa Gamma Chapter meeting because of the fatigue. By Day 15 I made it to my physical therapy session. On Day 16, I enjoyed a long breakfast out with a friend. On Saturday, Day 17 I was feeling strong enough to go to Monmouth for an all-day Delta Kappa Gamma State Leadership Conference. Fortunately, Melanie drove as I was tired by the end of the day. The fatigue came back. There were two Breast Cancer Support Group sessions during this cycle, Sept. 5 (Day 6) and Sept. 19 (Day 20.) I was able to make it to both sessions, and have been paying particular attention to those who talked about radiation and those who have been taking the anti-estrogen medications, long term. I still have both of these ahead of me. I meet with my oncologist, Dr. Acheson, on Sept. 28 to discuss the anti-estrogen meds I’ll start after radiation. On October 3 I go in to radiology for the “mapping” appointment where they set up everything so I am positioned exactly the same each time. I will start about a week later. I’m scheduled for twenty-five sessions; every weekday for five weeks. More on that after I get started. Paul has been such a trooper, doing all the cooking, dishes, watering plants, grocery shopping, etc. and never complaining. What a love!!! That sums up the last three weeks following my Fourth and Last chemo session. I made it through, like I knew I could. Yippee!!! No Regrets is still my motto. Living with AFib:
As an aside, you probably noticed that I keep referring to my heart going into AFib. I was asked how I can tell? Usually, the first thing I notice is that my heart is pounding noticeably in my chest. When I sense this, I use test #2 and have my Apple Watch take my pulse, which is an app I have readily available on it. Since my normal resting rate is somewhere in the 60s or low 70s, if it is bouncing around between the 80s and 110 bpm (sometimes as high as 134), I have a pretty good idea I am in AFib. Then there is test #3. This is to use a little EKG recorder a friend told my about. It is made by Kardia and I got it on Amazon for $99. It pairs with an App by the same name that I have on my iPhone. It has two metal plates onto which I place fingers from each hand. They connect over bluetooth and it takes a 30 seconds reading. I then email the results to myself as a PDF and print it out. When I asked my cardiologist, he said that a lot of his patients have them, and he totally approved. I can show a doctor the rhythm printout taken while the event is happening. What I am realizing, however, is that my heart probably goes in and out of AFib more often than I realize, which makes my very happy that I am on Eliquis blood thinner to avoid the clots/stokes that can be generated when your heart functions irregularly. My cardiologists are just trying to get me through all this cancer stuff, then will deal with my other heart issues. I know I’m eventually looking at a pacemaker, but not now. I have two cardiologists watching over me. If you, or any of your friends or relatives have issues with AFib, check this out: ActiveCor and have them consult their cardiologist to see if it is right for them. https://www.alivecor.com. |
AuthorGrace Pitzer Archives
December 2023
Archives
December 2023
Categories |






















































 RSS Feed
RSS Feed