End of Radiation and On With Life! Wow, what a year 2017 has been. It definitely had its high and low points, but the good thing is that it is ending on the up side.
To do a brief recap: the year started with our going to Green Valley, AZ in January followed by a two week trip to Cuba in February. That was when I discovered a lump in my armpit. The end of March I had it biopsied and it was diagnosed as a lobular carcinoma. Since we were scheduled to leave in two days for a two week photo expedition cruise around Baja, California, we were encouraged to go. It was a great distraction. (See photos under Photo Gallery menu above.) We returned to Green Valley then home to Portland in mid April when the whirlwind started. An MRI showed that I had several tumors in the breast on the other side, which the 3-D Mammogram did not show. So, on May 10 I had a double mastectomy. My cancer type was Estrogen Responsive Positive (ER+) and the Oncotype DX test showed that I would benefit from Chemo. I started the four sessions of chemo on June 28 and the last session was on August 31. I managed the side effects, which you can read about in previous posts. In October 13 I started radiation treatments. They were daily for 28 sessions, ending on November 20. (My November 4 Post tells the details of the sessions.) There were a couple of side effects. One was fatigue. Since I was already back to working out at Curves three days a week and walking three days, I found the fatigue minimal. The other effect was like a “sun burn.” I managed to keep that to a minimum by using two gels: Aloe Vera 99% and Calendula three times a day. After the last treatment I was given a prescription for 1% Silver Sulfadiazine Cream which is used on burns. I applied it thickly twice a day. Dr. Gannett, my radiation oncologist was always pleased with how well I was doing. I saw him on December 18, one month after my last treatment, and should not have to see him again. Meanwhile, on November 29 I met again with Dr. Acheson, my medical oncologist. She was pleased with how well I am doing. We had a discussion about what comes next. My type of breast cancer is Estrogen Responsive Positive (ER+.) This means it feeds on estrogen. Believe it or not, our bodies continue to produce estrogen after menopause, so it is important to shut down all of it. Therefore, there are various medications that are recommended to reduce the risk of the cancer re-occurrence. Since I do not have a bone density problem, I qualify for the class of drugs called Aromatase Inhibitors (AI.) Dr Acheson is starting me with Letrozole. It is important to be able to take one of these for at least five years. If I tolerate this one, great, if not there are two other AI drugs to try. I started December 1, and so far so good. Then there is my hair. It has now grown out to about an inch long. I can tell there will be some curl, at least for a while. It will be some weeks before I stop wearing something, hat, scarf or wig, because I’m cold otherwise. Then there is my heart issue: totally unrelated to my cancer. I continued to have occasional AFib episodes. I had a 48 hour Holter Monitor test which showed no pauses over 2 seconds. I also had an echo stress test (with treadmill) which shows my heart muscle is healthy. All Good News!!! Since I’m on the blood thinner Eliquis I don’t have to worry about blood clots and strokes, so until my AFib episodes get to be too frequent or of concern, I don’t need to have anything done about them. It is good that I have two cardiologists looking after me. About the time I started chemo I learned about the Breast Cancer Support Group sponsored by Providence St. Vincent, which meets twice a month. I have attended all but one session since then, and find them very helpful. I have been able to learn from others going through what I have, am or will go through. The women who run the sessions are also very helpful, and I plan to continue attending when I can. So, this ends the year 2017, and I’m so thankful that I have made it through all of these annoyances and blips to my health. I’m looking forward to the new year and getting back to “normal.” We look forward to returning to Green Valley, AZ for the winter where I have twelve classes already scheduled for me to teach at the Camera Club. I will post again in the future every once in a while to chronicle any changes, or to just let you know I’m doing fine. You can also check back periodically to see photos of our travels. That was the original purpose of my website, since travel and photography are my special interests. Until then, thanks for reading about my breast cancer journey. I hope it has been informative. May we all have a Happy New Year! Grace
0 Comments
Thank You: From My Sister Dear Special Friends of Grace,
Grace is my older sister. We've been together for many years ;0) She means the world to me. I would prefer to be the one to do all the things for her that I will mentioned. Since it was impossible for me to do all that, along came you folks, "Grace's Special Friends". "Thank you!" to each one of you for coming along side her, cheering, comforting, and doing whatever you did, to make her year bearable, enjoyable at times, and doable because you were there for her. I deeply appreciate what you have done and wanted you to know my observations as time went by and Grace's sense of well-being because you were there for her. This is Grace's last week-end before her last Radiation treatment, and then there is "recovery time." Some of you were with her from the beginning, making trips to the doctors, and taking notes which relieved her mind so she could focus on what was being said. Some of you took on the "Care-Giver" role. Some of you periodically provided transportation. Some of you cooked special meals, and brought them over for Paul and Grace. Some of you sent her flowers, cards, and your prayers and love. Some chose to wait in the waiting room during her surgeries. I know that Paul appreciated your support, as well. Some called to see how she was doing; and, my guess is, some of you checked on Paul to see how he was doing. I'm sure I left out some of your acts of kindness toward Grace. Grace is a wonderful sister to me and a great example for me to follow on this road of recovery. May each of you stay in good health for many years to come; and if not, may you be surrounded by the same kind of friends that you have been to Grace to help see you through. May God bless you as you have blessed others. Very Sincerely, Gayle Radiation: First Half of 28 Sessions I see that my last update was dated September 20, which seems like a long time ago. It was three weeks after my last chemo infusion. Since then all of my side effects have disappeared with the exception of my fuzzy/numb feeling toes. My strength has slowly returned and a couple weeks ago I realized that I really was feeling very NORMAL. For three weeks now I have been back to doing full workouts at Curves, three days a week, and walking the other three days of the week. This is all very good since fatigue is a normal side effect of radiation and so far, I have not experienced any!
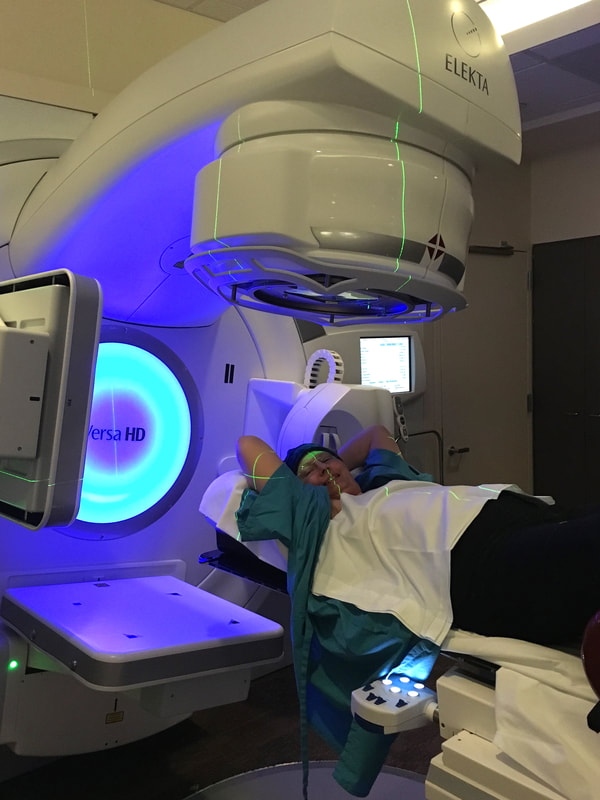
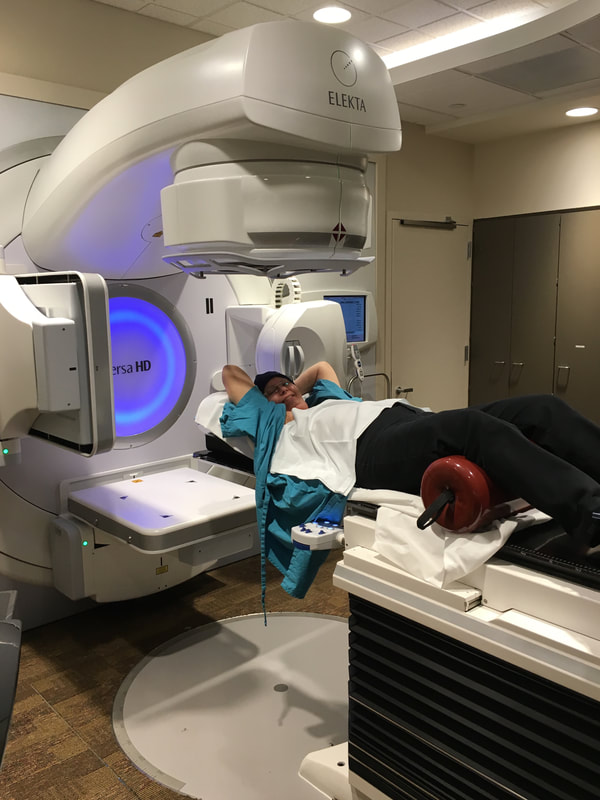
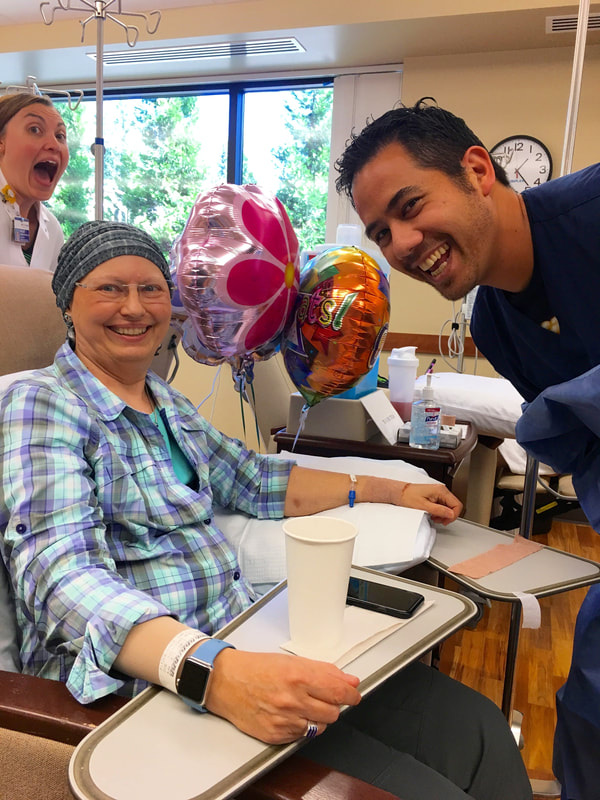
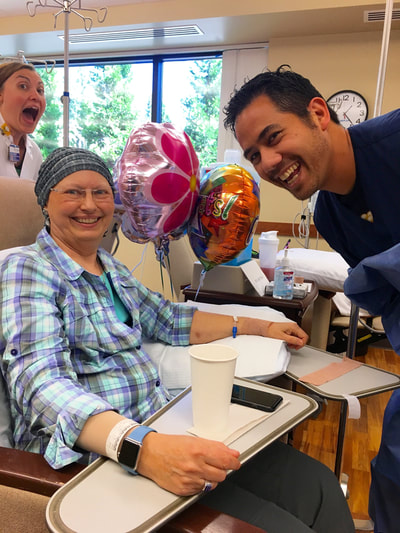
On October 3, I had the “mapping” for my radiation treatments. They made a mold of me in the right position so I can lay in it exactly the same each time. I started the 28 daily sessions on October 12. My regular appointment is 10:24 AM every day. I always go in early, just in case traffic is bad, and work on the group jigsaw puzzle they make available. The actual session only takes less than ten minutes, and the radiation from three angles is for 12, 10 and 19 seconds each. About day 12 my skin started to get a little pink. I have been faithfully using the recommended 99% Aloe Vera gel and Calendula gel three times a day. This is when it may be an advantage that much of the area is still numb from the surgery, so I’m not feeling many uncomfortable sensations. Every week they take X-Rays of me in position to make sure everything is still being set up correctly. Once a week I also see Dr. Gannett. He answers any questions I have and looks at my skin to see how it is fairing. So far, he is very pleased with how everything is going and how good my skin is tolerating the treatment. He is also surprised that I am not yet experiencing any fatigue, but attributes that to my continued exercising. One thing I learned in our discussion is that the side effects (fatigue and skin irritation) should be gone within three weeks of ending the radiation treatments. November 20 is the last one, so that means I should be in good shape by the second week in December, if not before. Also, my hair is growing back, but can still be measured in 1-2 mm. I'm trying to be patient and know it will take a couple more months to be presentable. In the mean time, my warm fleece stocking caps will have to do. On November 29 I meet again with my medical oncologist, Dr. Acheson, to discuss the anti-estrogen pills I will need to take for at least five years. I expect I’ll be starting them in early December. That can be the next blog post topic. It has been fifteen years since we have remained in Portland for the fall season, to enjoy all of the gorgeous foliage colors. We have missed that, so we are really enjoying colorful trees and the nice weather we have also had, up until this week. The rain has now hit. That doesn’t stop me from my walks, however, as I have plenty of rain gear. I finally did put a personal post on Facebook in honor of “Breast Cancer Awareness Month” to encourage everyone to get those annual mammograms. And, if the results come back with a “Too dense to be sure” comment, have a followup ultrasound, at least. I’ll make another update when the radiation is finished (11 more to go) and the extra three weeks the side effects could last. Happy Thanksgiving. Paul and I certainly have a lot to be thankful for; especially my getting back to good health!! Chemo: Session Four - THE LAST, August 31, 2017 On August 31 I had my LAST of four chemo infusions. Besides Paul, I was joined by my friends Melanie and Sarah. Melanie even brought balloons and cupcakes to celebrate the occasion. After my blood draw I met with Erin, the physician’s assistant, who reviewed my last three weeks, checked me over, and discussed any possible changes for the next three weeks. She did mention that the results of chemo is cumulative and the fourth could hit me a little harder. My blood work was good, so we all moved to the infusion room. Since it was lunch time by then, I sent everyone off for lunch while I took the Zofran anti-nausea pills and ate my own peanut butter and jelly sandwich along with some things I scrounged from the refrigerators. After the half hour wait for the Zofran to take affect I was hooked up to the Taxotere bag which took an hour to empty. Sometime during that hour everyone came back from lunch. Paul figured I was in good hands, as Melanie could take me home. Before he left, we got a group picture of my three supporters for the day. (see below) When it was time to switch to the Cyclophosphamide bag, which only required a half hour to empty, Sarah took a picture of me with my nurses for the day. (see below) They were all excited for me that this was my last visit. I was pleased that my friends cared enough to spend the time with me. However, I knew this wasn’t the end!!! I still had to endure the three plus weeks of side effects from the final chemo infusion. As I mentioned above, I was told the effects were cumulative, and she was right. They hit harder and faster. 1. Fatigue: Started Day 2 and I noted it was serious until Day 12 when it let up some and came back Day 18 and continues on to Day 21. Hopefully it will not last much longer. 2. Nausea: I took Compazine for nausea on Days 1, 2, 4, 5, and 9, mostly at night. I would take it if my stomach was even a little unsettled so I really never got sick. 3. Tender fingernails: Started Day 5 and lasted until Day 13. My thumbnails are growing out with ridges parallel to the cuticles and all my fingers have vertical ridges. They are very brittle so I keep them fairly short. 4. Feet: About Day 11 I realized my feet felt like I had on very fuzzy socks. When I looked, there were no socks. This has persisted until now, some days more so than others. Sometimes the soles of my feet have spasms, which don’t last long. This was a new side effect. 5. Mouth Sore: Starting Day 4 my tongue became sore, mostly the edges. By Day 6 the texture on the roof of my mouth became rough. This lasted at least a week or so. I rinsed with salt water to help. 6. Taste Changes: The sore mouth coincides with how things taste, including water. Food and water didn’t start tasting normal until after Day 13 and I noticed water tasting normal on Day 18. Finally I can enjoy eating and don’t mind drinking. 7. Atrial Fibrillation: I speculate that because of my extreme fatigue, staying on the sofa, and water not tasting good, I let myself get dehydrated. The night of Day 11 my heart went into AFib, which I noticed after I went to bed. I got up and took my blood pressure, which was low, and my heart rate was 101 bpm. I used my Kardia EKG device that connects to an App on my iPhone and took a 30 second reading, which confirmed my suspicion. I printed it for my records, drank some water and went back to bed. In the morning I started downing Gatorade for the electrolytes, and by noon my heart was back in normal rhythm. This left me even weaker, however. (See below titled “Living With AFib” to learn about this little EKG device and the App.) 8. Imodium: I only needed to use it once, on Day 11. 9. Prunes: I discovered they are my friend and almost daily consumption kept me from needing to use any Dulcolax. On Day 11, September 10, we had to miss a family wedding because of my extreme fatigue. It was later that night when the AFib started. The next evening I had to miss my Delta Kappa Gamma Chapter meeting because of the fatigue. By Day 15 I made it to my physical therapy session. On Day 16, I enjoyed a long breakfast out with a friend. On Saturday, Day 17 I was feeling strong enough to go to Monmouth for an all-day Delta Kappa Gamma State Leadership Conference. Fortunately, Melanie drove as I was tired by the end of the day. The fatigue came back. There were two Breast Cancer Support Group sessions during this cycle, Sept. 5 (Day 6) and Sept. 19 (Day 20.) I was able to make it to both sessions, and have been paying particular attention to those who talked about radiation and those who have been taking the anti-estrogen medications, long term. I still have both of these ahead of me. I meet with my oncologist, Dr. Acheson, on Sept. 28 to discuss the anti-estrogen meds I’ll start after radiation. On October 3 I go in to radiology for the “mapping” appointment where they set up everything so I am positioned exactly the same each time. I will start about a week later. I’m scheduled for twenty-five sessions; every weekday for five weeks. More on that after I get started. Paul has been such a trooper, doing all the cooking, dishes, watering plants, grocery shopping, etc. and never complaining. What a love!!! That sums up the last three weeks following my Fourth and Last chemo session. I made it through, like I knew I could. Yippee!!! No Regrets is still my motto. Living with AFib:
As an aside, you probably noticed that I keep referring to my heart going into AFib. I was asked how I can tell? Usually, the first thing I notice is that my heart is pounding noticeably in my chest. When I sense this, I use test #2 and have my Apple Watch take my pulse, which is an app I have readily available on it. Since my normal resting rate is somewhere in the 60s or low 70s, if it is bouncing around between the 80s and 110 bpm (sometimes as high as 134), I have a pretty good idea I am in AFib. Then there is test #3. This is to use a little EKG recorder a friend told my about. It is made by Kardia and I got it on Amazon for $99. It pairs with an App by the same name that I have on my iPhone. It has two metal plates onto which I place fingers from each hand. They connect over bluetooth and it takes a 30 seconds reading. I then email the results to myself as a PDF and print it out. When I asked my cardiologist, he said that a lot of his patients have them, and he totally approved. I can show a doctor the rhythm printout taken while the event is happening. What I am realizing, however, is that my heart probably goes in and out of AFib more often than I realize, which makes my very happy that I am on Eliquis blood thinner to avoid the clots/stokes that can be generated when your heart functions irregularly. My cardiologists are just trying to get me through all this cancer stuff, then will deal with my other heart issues. I know I’m eventually looking at a pacemaker, but not now. I have two cardiologists watching over me. If you, or any of your friends or relatives have issues with AFib, check this out: ActiveCor and have them consult their cardiologist to see if it is right for them. https://www.alivecor.com. Chemo: Session Three (of 4): August 9 - 31, 2017On August 9th I had my 3rd chemo infusion. By now I know the routine: show up, pick a chair, get the IV placed and have blood drawn. Melanie was back with us for this visit to act as my scribe. Next I saw Dr. Acheson, my medical oncologist, and we reviewed how everything went during the last session. Basically, I had the same side effects as the previous sessions. 1. Fatigue: started on Day 4 again and lasted until Day 11. 2.Tender fingernails: started Day 5 and ended Day 8. 3.Mouth sore: started Day 4 and ended about Day 9. No sore tonsil this time. 4.Taste changes: Not significant enough to note, but probably lasted about a week. 5.Didn’t Have: a fever or any AFib episodes. 6.Need for Imodium: Days 7 and 8. Discovered Prunes: I had forgotten about the prunes I bought before starting chemo. I started eating some daily with breakfast on Day 18 and that eliminated the need for Dulcolax. On August 10, the day after my infusion, I attended a morning session called “Look Better, Feel Better” put on by the American Cancer Society. They provided a whole packet of beauty and make-up products and the representative went through them all, showing us how to apply each one. It was fun, and I went away all made-up to attend a play at our local Lakewood Theater that night. The steroid, Dexamethasone, I have to take twice a day the day before, day of, and day after my infusion causes insomnia. By Friday and Saturday I was pretty exhausted. That just leads into my fatigue sequence of days. I did attend the one Support Group during this time. It was a smaller group, but interesting, and I’ll return next month. The big event here in our area was the solar eclipse on August 21. We were invited to spend the time at my cousin and husband’s (Linda and Richard) place in Lincoln City on the Oregon coast, and within the area of Totality. To avoid the predicted heavy traffic going to the totality areas we drove there on Friday. We think the weather and traffic predictors scared many people away, as neither dire predictions came about. Monday morning, Aug. 21, dawned with some fog a short ways inland, but by eclipse time, about 9:00 am, it had pulled back to the beach, giving us a full view of the eclipse. I set up my tripod and camera in a driveway across the street. I used a “White light solar filter” attached to the lens. For those of you interested, I was using my Canon 70-200mm lens with a 1.4X extender attached to my Canon 7D DSLR that has a crop sensor (X 1.6) which gave me a total zoom of 448mm. I got fair shots but missed the diamond effect as I was busy putting the filter back on the lens. Ugh! The picture below is a composite of some of my shots as the eclipse progressed. Fortunately, the eclipse was on my Day 13 when my energy level was beginning to return. We returned to Portland the next day, managing to avoid some of the heavy traffic. On Days 15, 17 20 and 22 I felt like going to Curves to exercise. I am still just doing the circuit one, instead of the usual twice, and doing all the stretches. It feels good to be back. My LAST, #4, infusion was yesterday, August 31. All went well and along with Paul and Melanie another friend, Sarah, joined us to help celebrate the event. I will write about it, and how everything went for the final three weeks sometime around September 20. (See pictures below.) My Radiation is scheduled to start October 10: every day for five weeks. More on that later. I am still staying positive and happy with all my decisions. We are both looking forward to celebrating the end to it all by Thanksgiving and Christmas, and looking forward to getting back to Green Valley, Arizona mid January. Remember that my motto is still “No Regrets.” My favorite aria by Edith Piaf. Click on each picture to enlarge.
Chemo: Session Two: July 19 - August 8, 2017 For a quick review, my chemo is scheduled in four sessions or cycles, each three weeks apart. My first was June 28 and the second on July 19. The last two will be on August 9 and 31.
On July 19, I received the second infusion of the two drugs, Taxotere and Cyclophosphamide. Since Melanie was out of town, my friend Jan joined Paul and me to act as our scribe and just be there for moral support. The routine was the same: IV and blood draw, visit with physicians’ assistant, Erin, to cover the first session, and on to the infusion. All went smoothly. During this second cycle some of the side effects hit more quickly and lasted a little longer. 1. Fatigue: started on Day 4 and didn’t let up until Day 12. 2. Tender finger nails: started Day 5 and lasted until Day 10. 3. Mouth sore: started Day 4 and lasted until Day 13. 4. Sore tonsil: same as last time, and lasted until Day 13. 5. Fever - new: Day 10 I was cold and my temp went from 100 at 11:00 am to 101.8 at 7:30 pm. a. Called the doctor and after eliminating anything viral was prescribed an antibiotic. b. Temp returned to normal by Day 12. 6. Taste change - new: part of time between Day 4 and 13 food started tasting different. a. Had to force myself to eat. b. Added some Gatorade to water so it didn’t taste bad. As a result of the fever, happening on my low energy days, we had to miss the 50th Anniversary celebration of our good friends Iran and Fran. We also missed the going away picnic for our goddaughter, Molly, who is moving to Honolulu where she will be doing her doctoral residency. We were able to walk three doors down to attend our neighbors’ open house, though, so the whole weekend wasn’t a total wash. By Day 13 I was feeling pretty good and the rest of the 21 days were good ones. I was able to go to Curves several times and even go shopping a few times. The special day was being able to attend an all-day DKG meeting in Monmouth, and I felt completely normal. I must admit I needed rest the next day. Another positive outcome of this session 2 was that I did NOT have any more episodes of AFib. None! My cardiologist was very happy to hear that. He also commented that the Kardia EKG printouts I had from all the episodes during session 1 were very helpful (See a couple posts back where I talk about “Living with AFib.) The Breast Center at St. Vincent Hospital runs a support group which meets twice a month. I was able to attend the first time on August 1st. There were about fourteen who attended, plus the hospital volunteers. The group varied from a young lady who had just been diagnosed to some long term survivors. I was the only one currently in chemo, but several were in radiation and several were going through reconstruction. When it became my turn, I shared my motto of “No Regrets,” my Kardia EKG machine, and my system of tracking side effects. When it was all over, I was glad I went and will go back. My take-aways were: 1. I was very happy to have decided not to do reconstruction. 2. I was happy with all my decisions. 3. I felt very good about myself and my positive attitude. The American Cancer Society offers a session called “Look Better, Feel Better” which will be held August 10 at St. Vincent. I have signed up for it. I understand we are given some make-up and shown how to apply it, and other tips for looking good. Sounds like fun. Today, August 9, I had my third infusion, and all went well. My next post will be after I have completed this third session, sometime around August 31 - when I get my last infusion. In the meantime, I’m staying positive and enjoying life. Chemo: The Rest of Session One, with pictures Briefly, my chemo treatments will be in four doses, called infusions, administered three weeks apart. The first was on June 28 (followed by July 19, August 9 and 30.) My last blog post was about the first 10 days of session one. I have now completed the full 21 days. As predicted, my energy level hit its lowest point on days 10-12. I had experienced some soreness in my mouth, which I treated with salt water. That lasted about nine days, ending on day 14. There was some irregularity which I treated with either Imodium or Dulcolax, whichever was appropriate. The bouts of Atrial Fibrillation I talked about in the last post quit on day 12 and my energy level began to rise. At physical therapy on day 13 my therapist told me my range of motion was good enough that she would encourage me to go back to Curves for strengthening exercises. That felt like being given a prescription to “RESUME LIFE.” I went the next morning and it felt so good. I only did one round on all the machines and had no problems with any of them. I repeated that again on day 17. On day 14 I had an appointment at Just Like A Woman to pick up my “New Boobs” and be fitted for a bra, which has pockets to hold them. For whatever it is worth, I had decided to go down in size, although I can be any size I want to be. The hard part was finding a bra that didn’t cut too tightly into my armpits. Since my insurance company will pay for two sets of forms every two years, and three bras a year, I got two sets of forms, one being the sports type that I can use in the pool, etc. I went home with one bra and one on order. I can’t explain how much better and “normal” I feel while wearing them. Also, on day 14, my hair started coming out as I was washing it. This continued to happen each day, and more cane out when I combed it. I knew then that I would not make it to the family wedding on day 18 with my own hair, so I made an appointment with my hairdresser, Pam, to have it buzzed off (not shaved as that runs the risk of ingrown hairs.) Paul’s sister and brother-in-law were in town for the wedding on Saturday. Mary offered to go with me when I got my hair cut, which was very sweet and much appreciated. We turned it into a fun event. Pam suggested a Mohawk before it was all gone. She spiked it up and put green streaks in it for a picture. A friend later said I looked like “Every middle-school kid’s dream teacher.” My new wig was deemed good to go and my new scarves looked good, so I left a happy person, ready for my evening debut at that evening’s Condo Happy Hour and the wedding the next night. What could have been an emotional “downer” wasn’t!!!!! My energy level continued to be good right up to my second cycle infusion. I did have to pay attention to how many things I tried to do in one day, and budget my energy with some rest periods along the way. All in all, I have been exceedingly pleased with how the whole session/cycle one has gone. I fully realize that all this will be somewhat accumulative and that each of the next three cycles may have more symptoms develop. My second session was July 19, and everything went smoothly. I even went to Curves the next morning, but have to admit to more fatigue. The Physician’s Assistant I saw reviewed how everything had gone the first three weeks, which was normal, and we discussed more possible side effects that could come on after this session; none too daunting. Mainly the pattern will repeat, and I have kept good notes. My motto is still “No Regrets,” which is also my favorite aria sung here by Edith Piaf in English. A neighbor found this other version which you won’t want to miss. https://youtu.be/qxYpQ-jMe44 (embedded below) My next post will be after session 2, around August 9. Hugs, Grace Chemo: Session/Cycle One of Four I left off the last post having made a decision to go ahead with chemo because it would decrease my risk of a reoccurrence of the breast cancer by a few percentage points. I learned that the chemo formula for my Estrogen Receptor Positive (ER+) type of cancer (with only one lymph node involved) would be two drugs: Taxotere and Cyclophosphamide, known as TC. They are not as toxic as others and should not affect my heart at all.
Since I am only getting four infusions, each three weeks apart, they are not putting in any kind of a port. The day before my first infusion, I packaged up lunch, entertainment, snacks, etc. and had everything ready to go. I must have been more stressed than I realized, however, because my heart decided to go into Atrial Fibrilation again. I waited a couple of hours and then called both the oncologist’s office and my cardiologist. This was mainly to report in that it was happening. As always, it corrected overnight and I was good to go the next day. In preparation for the infusion, I was prescribed Dexamethasone, a steroid that counters some of the effects of the chemo and also suppresses nausea. I take it the day before, the day of, and the day after. Insomnia is a side effect, but that only lasted three nights. June 28, Session 1: I was to arrive at 11:00 to check in and have my blood drawn and tested. They want to know that all levels are acceptable. In the infusion room, I got to pick from several recliner-like chairs where I would spend my time that afternoon in full view of my nurse. Unfortunately, it took two tries and two people to get a good IV set, which was used for both the blood draw and the infusion. I have difficult veins. While waiting for the blood work results to come back from the lab we met with Dr. Acheson. I need to say right here that my friend Melanie was with us the entire time. She has been a god-send as she takes great notes, and I can read them afterward. The doctor shared more information and answered questions. When my blood work results were back she went over them as well. Turns out my white blood count was high, potassium, magnesium and sodium were low. None of that would hinder treatment, but I may need to make some diet changes. From there we went back to the infusion room. It is a large sunny room with many windows and a snack bar. I was given an anti-nausea medication and had to wait a half hour before the infusion could start. By then I was getting hungry and ate part of my cheese sandwich. Lunch for Paul and Melanie would have to wait. Nurse Liz came over and shared a bunch more information about the side effects I could expect, how to deal with them, etc., etc., etc. I was then hooked up to the first chemical (T). Then I sent Melanie and Paul off to the cafeteria to get their lunch. I had just set up my iPad to watch the movie “Turner and Hooch” when Matt, the pharmacist, came in to discuss all the medications. Fortunately, Melanie and Paul came back because I was having a hard time taking notes in a readable manner. Matt went over the anti-nausea medications that I picked up at the pharmacy a couple days before: Compazine and Zofran. The staff absolutely does NOT want me to get sick. There are also other over the counter medications we can use to control either diarrhea or constipation. They don’t want either of these to get out of control. All Paul and I had to do when we got home was pull out our travel kit for Imodium and Dulcolax - things we routinely carry on our travels. By 3:30 the last of the two chemo bags was empty, my IV was taken out, and I was released to go home. I felt fine. At home I had to take the steroid for one more day and it was recommended that I take Compazine for a couple days, just to be sure I didn’t get nauseous. Symptoms and the 21-day Cycle: I was told to keep track of all my symptoms over the following 21 days, because the pattern that developed would probably be repeated for all the cycles. Day 1 is the infusion day, which in my case will be on Wednesdays. I have printed out a “Weekly” calendar with times running down in columns. I am color-coding my medications and symptoms so I can see them at-a-glance. Possible Symptoms to watch for: 1. Low blood: assessed on day of infusion. 2, Fever: none 3. Nausea and vomiting: some unsettled stomach issues and took med. No vomiting. 4. Constipation and diarrhea: all controlled with occasional medication like Imodium or Dulcolax - depending on which one was needed. 5. Changes in appetite and taste: somewhat less appetite, everything still tastes good 6. Changes in mouth: slightly sore mouth, mostly when I get up in morning, handled with salt water wash and/or gargle 7. Changes to hair, skin and nails: no hair loss, no skin issues, fingernails are tender and sensitive to extra warm temperature 8. Fatigue: worst days were 4-6 and 10. Energy level should go up now after day 10 until day 21 and the cycle repeats. That is how it breaks out for the first 10 days of the 21 day cycle. If you know me, however, I like to plan ahead. So, I took advantage of checking out the free wig selection at the “Transitions” department, which St. Vincent has, and was able to find one that my hair dresser says is a great fit and color for me. The style is not that different from my own. Today, my cousin brought over her collection of scarves, hats, etc. from when she had breast cancer six years ago. With all of that in hand for a start, I’m hoping to be ready for any social event and about-the-house when/if my hair comes out. Hair loss will probably start sometime before my next cycle, but for sure after the next infusion. I’ll try to let you know how the final 14 days of this cycle go in the next post. Check back in two weeks. Living with AFib: As an aside, you probably noticed that I keep referring to my heart going into AFib. I was asked how I can tell? Usually, the first thing I notice is that my heart is pounding noticeably in my chest. When I sense this, I use test #2 and have my Apple Watch take my pulse, which is an app I have readily available on it. Since my normal resting rate is somewhere in the 60s or low 70s, if it is bouncing around between the 80s and 110 bpm (sometimes as high as 134), I have a pretty good idea I am in AFib. Then there is test #3. This is to use a little EKG recorder a friend told my about. It is made by Kardia and I got it on Amazon for $99. It pairs with an App by the same name that I have on my iPhone. It has two metal plates onto which I place fingers from each hand. They connect over bluetooth and it takes a 30 seconds reading. I then email the results to myself as a PDF and print it out. When I asked my cardiologist, he said that a lot of his patients have them, and he totally approved. I can show a doctor the rhythm printout taken while the event is happening. What I am realizing, however, is that my heart probably goes in and out of AFib more often than I realize, which makes my very happy that I am on Eliquis blood thinner to avoid the clots/stokes that can be generated when your heart functions irregularly. My cardiologists are just trying to get me through all this cancer stuff, then will deal with my other heart issues. I know I’m eventually looking at a pacemaker, but not now. I have two cardiologists watching over me. If you, or any of your friends or relatives have issues with AFib, check this out: Alivecor and have them consult their cardiologist to see if it is right for them. https://www.alivecor.com. That is it for a couple of weeks. I am remaining positive and looking forward to the next 14 days with more energy. Paul's sister and brother-in-law are due to arrive on July 15 for over a week. We all have a family wedding we are looking forward to attending. Please feel free to leave a comment. I do get them and read them. ;-) I love hearing from my friends via e-mail, text, or phone. Next infusions are July 19, August 9, and August 30. Hugs, Grace Decisions, Decisions, Decisions - Ugh In my last post I covered my surgery - a bilateral (double) mastectomy which I call a quadruple mastectomy because it included the axillary ectopic breast tissue in each armpit. My recovery went smoothly and I regained strength every day, and I continue to work on range of motion. Many areas are still numb, and may be for a long time.
Now on to the "Treatment" phase. Dr. Ulloth had recommended radiation because there were so many (4) tumors in my right breast and the lymph node with a spot that had broken open was on the right side. On June 13 I met with my radiation oncologist, Dr. Christine Cha. It turned out she was very familiar with me because she was on the Breast Board when Dr. Ulloth presented my case. She very methodically went over all the reasons why I would benefit from having the radiation treatment on the right side, and that it would not affect my heart. There would be 25 sessions scheduled five days a week for five weeks. The actual radiation would only be about a minute, with getting ready and getting back dressed would make it about 15 minutes. This, of course, would take place after chemo, if I would be having that. For all of our doctors' appointments we have been taking our good friend Melanie to act as a "scribe." There is just too much information contained in the discussions to be able to try to take notes ourselves. I always go into an appointment with a list of questions. She makes sure we have covered all of those, but there are many other things in the rapid conversations with the doctor that could get forgotten or miss-remembered if it wasn't for her excellent notes. I highly recommend taking a scribe with you if you are having these kinds of doctor's appointments. On June 21 we met with my medical oncologist, Dr. Anupama Kurup Acheson. She was delightful and full of all kinds of information. She will manage several stages of treatment, chemo if I have it and the hormone treatment for years. Eventually we got to the results of that Oncotype DX test that would determine the need for chemo or not. As I had dreaded, the results were not clean. My score came in at 27 on a scale to 50. Right in the middle. UGH! Now I would have to make a decision. The risk of reoccurrence was 16% when only using the hormone suppressing medication like tamoxifen or aromatase. It would to down to 13% if I did chemotherapy. Making this decision would be hard, but when I learned what would be involved it didn't sound so horrible. There would be only two chemicals that would not affect my heart. There would be only four infusion sessions three weeks apart. I would get all kinds of anti-nausea meds, and one of the main side effects would be fatigue. I should be able to feel pretty good for half the time between session. Since the outcome of this test was what I had been dreading, having to make the decision, I had already done the worrying. If it will increase my odds of long term survival, I was willing to go for it. Paul, Melanie and I talked about it. The last question I had for Dr. Acheson was "What would you recommend your mother do if she was in my position." Her response was "Try it at least once." That gave me the feeling that there would be an out if needed. I appreciated that response. Also, when I told her I had gone from "Interesting" to "Complicated" and was going to use the word "Complex" for this next stage, she looked me straight in the eye and said, "You are a very nice person, but you aren't that special. You are right there with what we do every day." I guess that was quite a relief as well. On the way out I scheduled the first three sessions and then was shown the infusion room where I would come four times. There were comfortable recliners and a snack area with lots of things to eat and drink. I could have someone with me and bring in food and my own entertainment. Doable. Once home, I read through the chemo section of the books I've been using as references: Just Get Me Through This! A Practical Guide to Coping with Breast Cancer by Deborah A. Cohen and Robert M. Gelfand, MD and Dr Susan Love's Breast Book by Susan M. Love, MD, Sixth Edition 2015. Of course I had many more questions, and called the doctor's office to get them answered. The triage nurse, Holly, called me back and spent time answering them all. Then she put me in touch with the nurse navigator, Julie. She was very helpful and had lots more information and tips. I'm feeling much better about the decision. So, I'm set for the next phase of my recovery; chemotherapy. My infusion dates will be June 28, July 19, August 9 and 30. Radiation will follow after a few weeks recovery. In the mean time, since I have chosen to not do reconstruction, I need to so something to make me still look a bit more feminine. My friend Melanie and I went "Boob and Bra" shopping the other day. I will eventually find just the right combination and the sales lady was an excellent fitter. She has ordered some things that should work perfectly for me. All of this goes together with my theme or motto that I want to look back, in the future and say I have "No Regrets." It turns out that my favorite aria sung by Edith Piaf is "No Regrets." Listen to this beautiful auria. English Version Surgeries, Pathology and Recovery My last post left off with my surgery scheduled for May 10, 2017. It was to be a double mastectomy and also removal of the ectopic breast tissue on both sides. The afternoon before surgery I went to the hospital to have the dye injected into both breasts which would allow the lymph nodes' locations to show up during surgery.
May 10 I checked in at St. Vincent Hospital at 5:00 am and it wasn't long before I was taken back to the "Short Stay" surgery area and given a small room just large enough for the bed and a chair. There were many things done to prep me for surgery. I was also visited by the anesthesiologist, Dr. Ghode and by my surgeon, Dr. Ulloth. We discussed what she would be doing during surgery and she then had me sit up so she could use her permanent marker pen to draw the areas where she would make incisions and the sections she would be removing. At 7:30 am I was wheeled out to surgery. It took about 5 1//2 hours and at that time, while I was in recovery, Dr. Ulloth went out to tell Paul (and Alberto who had come to sit with Paul) that all had gone well and the lymph nodes were negative. That was a huge sigh of relief. It did not take long before I was out of recovery and back to the small room where I would spend the night. I tolerated the anesthesia and the pain meds I was receiving and did not get sick at any time. This sped up my recovery and I felt lucid and conversational very quickly. Because I had been advised not to be a hero, I took the pain medications when they were offered, which included both oxicodone and Tylonol every three to four hours. The night went well and I slept, using my own CPAP machine. The second day I enjoyed breakfast and lunch while waiting for the doctor to come by in the early afternoon and give approve my discharge. Back home I went directly upstairs to our family room where the big leather recliner is located. This would be my "bed" for some time to come, until I can use my arms well enough and can sleep on my side. I continued on the heavy medication regiment for almost a week. Six days after surgery, May 16, I saw Dr. Ulloth to have the bandages removed and the drain tubes taken out. Since the pathology report had not yet been posted, she made phone calls and talked to the pathologist. That is when I went from "Interesting" to "Complicated." That word kept coming into the conversation. It turned out that the one lymph node she had removed on my right side had in fact a malignant spot on it, which had broken open. At that time we all agreed that she had to go back in to get more nodes to make sure nothing had spread farther down the line. The next surgery was scheduled for the following Wednesday, May 24 when she would go back in through the same incision in my right armpit. Surgery number 2 took place May 24, again in the first time slot of 7:30 am. For this one, my friend, Melanie, was back in town to be with Paul. I was only in surgery a little over an hour and it went well, again. By noon I was in the car and we were heading home. This time I only took a few heavy pain meds for a couple of days, then Tylenol for a couple more. Through all of this, the only parts that hurt were the incisions across my armpits. The original one on my left side continues to bother the most. I was assured that with time that would improve. When I had the single drain tube from the second surgery taken out during an office visit on May 30, the pathology report had not been finished on those last nodes. Everything else was looking good. I made my final visit appointment for June 5. After she had inspected everything and removed the last lingering seri-strips Paul finally asked the big question. What was the result of the pathology report. ALL OF THE NODES HAD BEEN NEGATIVE!!! There was an audible sigh of relief from all of us. One last test was ordered. It is the Oncotype DX test which looks at 21 different possible gene mutations for my type of cancer, the Estrogen Responsive Positive, all others negative. The score from this test has a high ability to predict risk of re-occurrence and whether or not chemotherapy will be helpful or not. This test will take about two weeks. We said a final farewell to Dr. Ulloth and wished her well on her upcoming African Safari and retirement. I have appointments made with Dr. Christine Cha, a radiation oncologist; Dr. Acheson, a medical oncologist; and Jennifer Batchelor for a physical therapy assessment. |
AuthorGrace Pitzer Archives
December 2023
Archives
December 2023
Categories |
















 RSS Feed
RSS Feed