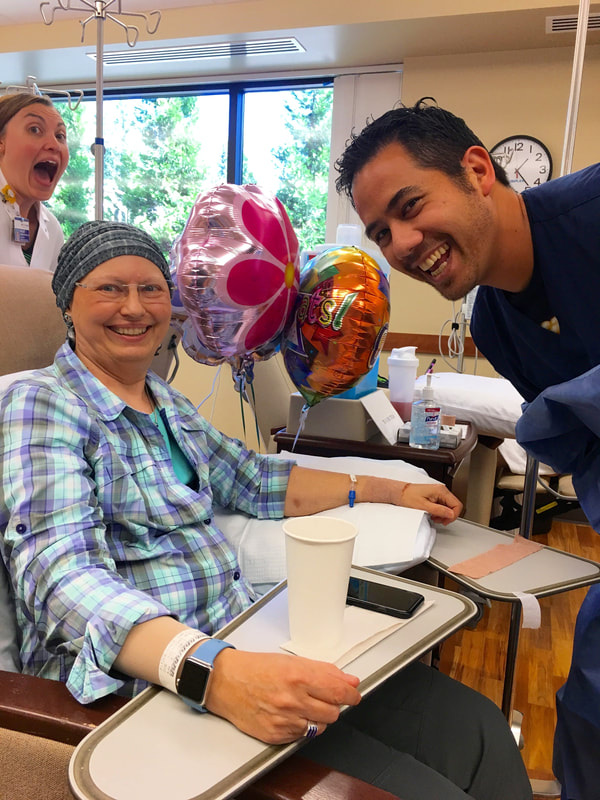
Chemo: Session Four - THE LAST, August 31, 2017 On August 31 I had my LAST of four chemo infusions. Besides Paul, I was joined by my friends Melanie and Sarah. Melanie even brought balloons and cupcakes to celebrate the occasion. After my blood draw I met with Erin, the physician’s assistant, who reviewed my last three weeks, checked me over, and discussed any possible changes for the next three weeks. She did mention that the results of chemo is cumulative and the fourth could hit me a little harder. My blood work was good, so we all moved to the infusion room. Since it was lunch time by then, I sent everyone off for lunch while I took the Zofran anti-nausea pills and ate my own peanut butter and jelly sandwich along with some things I scrounged from the refrigerators. After the half hour wait for the Zofran to take affect I was hooked up to the Taxotere bag which took an hour to empty. Sometime during that hour everyone came back from lunch. Paul figured I was in good hands, as Melanie could take me home. Before he left, we got a group picture of my three supporters for the day. (see below) When it was time to switch to the Cyclophosphamide bag, which only required a half hour to empty, Sarah took a picture of me with my nurses for the day. (see below) They were all excited for me that this was my last visit. I was pleased that my friends cared enough to spend the time with me. However, I knew this wasn’t the end!!! I still had to endure the three plus weeks of side effects from the final chemo infusion. As I mentioned above, I was told the effects were cumulative, and she was right. They hit harder and faster. 1. Fatigue: Started Day 2 and I noted it was serious until Day 12 when it let up some and came back Day 18 and continues on to Day 21. Hopefully it will not last much longer. 2. Nausea: I took Compazine for nausea on Days 1, 2, 4, 5, and 9, mostly at night. I would take it if my stomach was even a little unsettled so I really never got sick. 3. Tender fingernails: Started Day 5 and lasted until Day 13. My thumbnails are growing out with ridges parallel to the cuticles and all my fingers have vertical ridges. They are very brittle so I keep them fairly short. 4. Feet: About Day 11 I realized my feet felt like I had on very fuzzy socks. When I looked, there were no socks. This has persisted until now, some days more so than others. Sometimes the soles of my feet have spasms, which don’t last long. This was a new side effect. 5. Mouth Sore: Starting Day 4 my tongue became sore, mostly the edges. By Day 6 the texture on the roof of my mouth became rough. This lasted at least a week or so. I rinsed with salt water to help. 6. Taste Changes: The sore mouth coincides with how things taste, including water. Food and water didn’t start tasting normal until after Day 13 and I noticed water tasting normal on Day 18. Finally I can enjoy eating and don’t mind drinking. 7. Atrial Fibrillation: I speculate that because of my extreme fatigue, staying on the sofa, and water not tasting good, I let myself get dehydrated. The night of Day 11 my heart went into AFib, which I noticed after I went to bed. I got up and took my blood pressure, which was low, and my heart rate was 101 bpm. I used my Kardia EKG device that connects to an App on my iPhone and took a 30 second reading, which confirmed my suspicion. I printed it for my records, drank some water and went back to bed. In the morning I started downing Gatorade for the electrolytes, and by noon my heart was back in normal rhythm. This left me even weaker, however. (See below titled “Living With AFib” to learn about this little EKG device and the App.) 8. Imodium: I only needed to use it once, on Day 11. 9. Prunes: I discovered they are my friend and almost daily consumption kept me from needing to use any Dulcolax. On Day 11, September 10, we had to miss a family wedding because of my extreme fatigue. It was later that night when the AFib started. The next evening I had to miss my Delta Kappa Gamma Chapter meeting because of the fatigue. By Day 15 I made it to my physical therapy session. On Day 16, I enjoyed a long breakfast out with a friend. On Saturday, Day 17 I was feeling strong enough to go to Monmouth for an all-day Delta Kappa Gamma State Leadership Conference. Fortunately, Melanie drove as I was tired by the end of the day. The fatigue came back. There were two Breast Cancer Support Group sessions during this cycle, Sept. 5 (Day 6) and Sept. 19 (Day 20.) I was able to make it to both sessions, and have been paying particular attention to those who talked about radiation and those who have been taking the anti-estrogen medications, long term. I still have both of these ahead of me. I meet with my oncologist, Dr. Acheson, on Sept. 28 to discuss the anti-estrogen meds I’ll start after radiation. On October 3 I go in to radiology for the “mapping” appointment where they set up everything so I am positioned exactly the same each time. I will start about a week later. I’m scheduled for twenty-five sessions; every weekday for five weeks. More on that after I get started. Paul has been such a trooper, doing all the cooking, dishes, watering plants, grocery shopping, etc. and never complaining. What a love!!! That sums up the last three weeks following my Fourth and Last chemo session. I made it through, like I knew I could. Yippee!!! No Regrets is still my motto. Living with AFib:
As an aside, you probably noticed that I keep referring to my heart going into AFib. I was asked how I can tell? Usually, the first thing I notice is that my heart is pounding noticeably in my chest. When I sense this, I use test #2 and have my Apple Watch take my pulse, which is an app I have readily available on it. Since my normal resting rate is somewhere in the 60s or low 70s, if it is bouncing around between the 80s and 110 bpm (sometimes as high as 134), I have a pretty good idea I am in AFib. Then there is test #3. This is to use a little EKG recorder a friend told my about. It is made by Kardia and I got it on Amazon for $99. It pairs with an App by the same name that I have on my iPhone. It has two metal plates onto which I place fingers from each hand. They connect over bluetooth and it takes a 30 seconds reading. I then email the results to myself as a PDF and print it out. When I asked my cardiologist, he said that a lot of his patients have them, and he totally approved. I can show a doctor the rhythm printout taken while the event is happening. What I am realizing, however, is that my heart probably goes in and out of AFib more often than I realize, which makes my very happy that I am on Eliquis blood thinner to avoid the clots/stokes that can be generated when your heart functions irregularly. My cardiologists are just trying to get me through all this cancer stuff, then will deal with my other heart issues. I know I’m eventually looking at a pacemaker, but not now. I have two cardiologists watching over me. If you, or any of your friends or relatives have issues with AFib, check this out: ActiveCor and have them consult their cardiologist to see if it is right for them. https://www.alivecor.com.
0 Comments
Leave a Reply. |
AuthorGrace Pitzer Archives
December 2023
Archives
December 2023
Categories |

 RSS Feed
RSS Feed